Essential Guidance for Quality Improvement
Royal College MOC Supports QI Implementation
In collaboration with partners and stakeholders across the health care system, the Royal College is evolving its Maintenance of Certification (MOC) Program to integrate quality improvement (QI) and physician lifelong learning1,2,3. In small, practical increments, this renewed CPD strategy aims to be more relevant, improvement-focused, and user-friendly, enabling physicians to achieve care outcomes and/or continued personal-professional growth important to them and their patients.
Some specialists may be unfamiliar with QI principles4 and thus have difficulty connecting them to important improvement work they already do. Others might be challenged with identifying how to apply QI towards a specific personal development goal, professional practice role (e.g. clinician, educator, administrator) or during a career transition.
The following guidance aims to address these issues and provides
- an introduction to understanding QI science;
- tools, resources, and illustrative examples to help make connections between QI and existing professional practice;
- help to start planning, implementing, and reporting new QI initiatives in current professional practice; and
- direction on how to claim QI activities for MOC Program Section 3 (3 credits per hour).
What is QI?
What is QI?
New to QI and need a brief introduction? Maybe you’d like to know how this Essential Guidance to Quality Improvement fits in the current MOC Program. This section introduces the model for improvement (MFI) and its guiding questions to get you started.
Definition:
Quality improvement (QI) is a generic, robust, and action-oriented problem solving framework that supports you in elevating the current state of your practice, personal, or professional development. Depending where you want to focus improvement efforts, it may mean, for example, improving the delivery of patient and family care, your own mental health, delivering a more effective curriculum, and/ or using resources wisely.
The first part is about you, your team, and/or your health system assessing an area that needs improvement and establishing an aim.
Once you have identified the area of need, the next part is setting a plan of action in motion with the goal of improving the quality of either a process or outcome. For example, reflecting on the outcomes, and planning a course of action to continue the delivery of better patient care are critical pieces in ensuring quality care 5.
Videos:
Quality Improvement in Healthcare
A Good First Step to Any Improvement Project
Summary: In this 4-minute animated video, Dr. Don Goldmann explains the first step of quality improvement – Finding an aim and problem worthy of your QI efforts. Determining what ticks people off about their practice environment can be key to creating your problem statement.
What is the Model for Improvement and the PDSA cycle?
Familiar with the PDSA cycle? If you have been using MOC Section 3 activities in your professional practice, you have likely already been engaging in quality improvement.
Developed by Associates in Process Improvement, the Model for Improvement (MFI) is the most widely used QI model in health care 5. The MFI starts with you asking yourself three guiding questions that are then used as you test change interventions during various PDSA (Plan, Do, Study, Act) cycles.
The three guiding questions are 5,6
What are we trying to accomplish?
What problems are you addressing?
What do you know about your problem?
What evidence exists around the problem?

How will we know that a change is an improvement?
Change to process or outcome?
What domain of quality are you measuring? (i.e. safety, timeliness, effectiveness, efficiency, equitability, patient-centeredness)

What changes can we make that will result in improvement?
What solutions are you exploring?
What evidence do you have that this solution will address your problem?

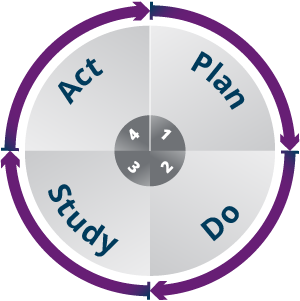
Sample: PDSA Cycle Implementation
What area of practice gets you excited to further examine and improve? The table below provides an example of a quality improvement PDSA cycle from planning to acting.
PROBLEM:
Trocar placement for laparoscopic cholecystectomy leads to reduced visualization and trocar clashing.
AIM:
Improve trochar placement technique.
MEASURES:
Initial optimal placement prevents operative complications by improving visualization.
| STEP | ACTION | EXAMPLES |
|---|---|---|
| PLAN | FORMULATE THE PLAN
|
|
| DO | EXECUTE THE PLAN
|
|
| STUDY | ANALYZE DATA
|
|
| ACT | QI PLAN MODIFICATIONS - WHAT'S NEXT?
|
|
Adapted From Taylor et al. 2014 7 | ||
Resources and Tools
QI within Residency Education
Do you want some guidance on how to embed QI within Residency Education?
Specialist eCoach
An online quality improvement tool created for specialists, by specialists, that guides you through the process of self-assessment, creating an action plan, evaluating results, and applying them to enhance your practice.
Choosing Wisely Canada
Looking for best practice standards to help inform your QI plan? Choosing Wisely Canada helps you find an MFI improvement aim or quality outcome to target. This collection of toolkits also provides evidence-based guidelines to help determine and change existing processes. Fully searchable by specific specialty, QI problem or outcome targets (e.g. early catheter removal, safe opiate prescribing) this web resource can assist your clinical QI implementation and evaluation plan.
If you are creating and implementing an improvement plan through Choosing Wisely, you can receive MOC Section 3: Practice Assessment for 3 credits per hour.
Reflective Exercise for Quality Improvement (QI) Initiatives
Completed a COVID-19 practice improvement change and looking to better organize or report it using a quality improvement lens? Developed by Royal College Fellows, this reflective tool helps you describe the practice change and quality domains targeted, in addition to listing data indicators used to measure improvements. Document how you used QI to improve practice in response to the COVID-19 pandemic and receive MOC Section 3: Practice Assessment for 3 credits per hour.
Annual Performance Review and Feedback
Undergoing an annual performance review and receiving feedback on your professional practice? Annual reviews provide physicians with an opportunity to reflect on past performance goals and establish plans for the coming year.
They can be a great source of data to identify potential QI gaps to target or even highlight any practice strengths you want to stay current with and continually improve upon towards mastery.
The entire process of reviewing this feedback, identifying future learning opportunities, and developing a proposed plan for continuous improvement of your professional practice is applicable under MOC Section 3: Annual Performance Review for 3 credits per hour.
Chart Audit and Feedback
How many of your patients with diabetes mellitus are appropriately referred for their annual eye exams? Questions like this are a great starting point for seeking and obtaining feedback from others via chart audit activities.
Chart audit and feedback is an assessment strategy that uses data recorded in a chart or electronic health record to assess the performance of an individual, group or team against one or more measures of performance.
The feedback provided during a chart audit establishes baseline data and can inform the identification of areas for future learning and quality improvement.
The entire audit process of identifying possible opportunities and listing desired quality improvement outcomes can be recorded under MOC Section 3: Chart Audit and Feedback for 3 credits per hour.
Direct Observation and Feedback
Have a trusted clinical peer whose opinion you value? Ever think about soliciting patient feedback on your discharge teaching or getting a colleague to scrub in, observe, and provide some coaching feedback while you do a lap chole?
Direct observation uses supervisors, colleagues or peers to observe a physician performing a regular professional activity to identify whether specific behaviours or competencies were demonstrated.
The coaching feedback provided during direct observation can facilitate the identification of areas for future learning and quality improvement.
Physicians being observed can record the time spent on the entire process, including identifying the outcomes for learning or practice improvements, under MOC Section 3: Direct Observation for 3 credits per hour.
Feedback on Teaching
Supervising residents in your clinic, teaching an undergrad course, or simply presenting at morbidity and mortality rounds this month? Consider using the Feedback on Teaching tool to summarise evaluations of your teaching completed by students, residents, physicians or health professionals to provide evidence related to the effectiveness and impact of your teaching.
Reviewing these evaluations provides opportunities to identify areas for improvement within this dimension of professional practice.
Time spent on the entire process, including identifying the quality outcomes for learning or practice improvements, can be claimed under MOC Section 3: Feedback on Teaching for 3 credits per hour.
Practice Assessment and Feedback
Reflect on why a patient consultation or procedure went really well or perhaps poorly. What data indicated the good or negative outcome? If you could start again, what would you do again and what processes would you change?
Practice Self-Assessment provides an opportunity to evaluate aspects of your daily work and target quality improvement aims across a variety of CanMEDS Roles. This type of self-assessment is not only for clinical setting and skills, but can be completed for all practice environments (e.g. academic and administrative).
Provided feedback is received, you can record the time spent on the entire process, including identifying the outcomes for learning or practice improvements under Section 3 Practice Assessment for 3 credits per hour.
Additional Resources
Quality improvement implementation story
How to claim MOC credit for everyday improvement projects (even in a pandemic)
Dr. Brian Wong & Dr. Lynfa Stroud share a close-call exposure to COVID-19 at work, what they did about it and tips for bringing a QI mindset to daily problem-solving.
https://newsroom.royalcollege.ca/how-to-claim-moc-credit-for-everyday-improvement-projects-even-in-a-pandemic/
Royal College Fellow Dr. Henry Bi explains how his team continually improved grand rounds, lessons learned, and connections to reporting this QI initiative in the MOC framework.
https://newsroom.royalcollege.ca/how-improving-grand-rounds-lowered-silos-in-our-faculty/
MOC Framework (where to report what QI activity)
Chart Audit implementation tips
The American Academy of Family Physicians provides some insightful direction on completing a QI chart audit in your practice setting
Choosing Wisely Canada integrated with QI
This example from the BC Patient Safety and Quality Council shows how best practice guidelines, the MFI model, and various PDSA testing cycles are implemented along the way to improving patient outcomes related to diagnostic imaging.
References
- Wong, B. M., Baum, K. D., Headrick, L. A., Holmboe, E. S., Moss, F., Ogrinc, G., ... & Frank, J. R. (2020). Building the bridge to quality: an urgent call to integrate quality improvement and patient safety education with clinical care. Academic Medicine, 95(1), 59-68.
- Levinson, W., & Wong, B. M. (2021). Aligning continuing professional development with quality improvement. CMAJ, 193 (18), E647-E648.
- Campbell, C., & Sisler, J. (2019). Supporting learning and continuous practice improvement for physicians in Canada: a new way forward. Summary report of the future of medical education in Canada (FMEC) CPD project.
- Yousefi, V., Asghari-Roodsari, A., Evans, S., & Chan, C. (2020). Determinants of Hospital-based Physician Participation in Quality Improvement: A Survey of Hospitalists in British Columbia, Canada. Global Journal on Quality and Safety in Healthcare, 3 (1), 6-13.
- Agency for Healthcare Quality. (2013). Module 4. Approaches to Quality Improvement. AHRQ. https://www.ahrq.gov/ncepcr/tools/pf-handbook/mod4.html
- Institute for Healthcare Improvement. (2021). How to Improve. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx
- Taylor, M.J., McNicholas, C., Nicolay, C., Darzi, A., Bell, D. and Reed, J.E., (2014). Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ quality & safety, 23 (4), pp.290-298.
- National Library of Medicine. (2021). Finding and using health statistics: Health data sources https://www.nlm.nih.gov/nichsr/stats_tutorial/section3/index.html
- Agency for Healthcare Quality. (2018). Data Sources for Health Care Quality Measures. https://www.ahrq.gov/talkingquality/measures/understand/index.html
- Centers for Medicare and Medicaid Services. (2020). CMS measures management systems blueprint https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/MMS-Blueprint

 Read more…
Read more…