Creating a Culture of Wellness in Medicine
Recommendations from the Royal College Physician Wellness Task ForcePRACTICAL, EVIDENCE-INFORMED RECOMMENDATIONS TO CREATE A CULTURE OF PHYSICIAN WELLNESS
What are the report outcomes?
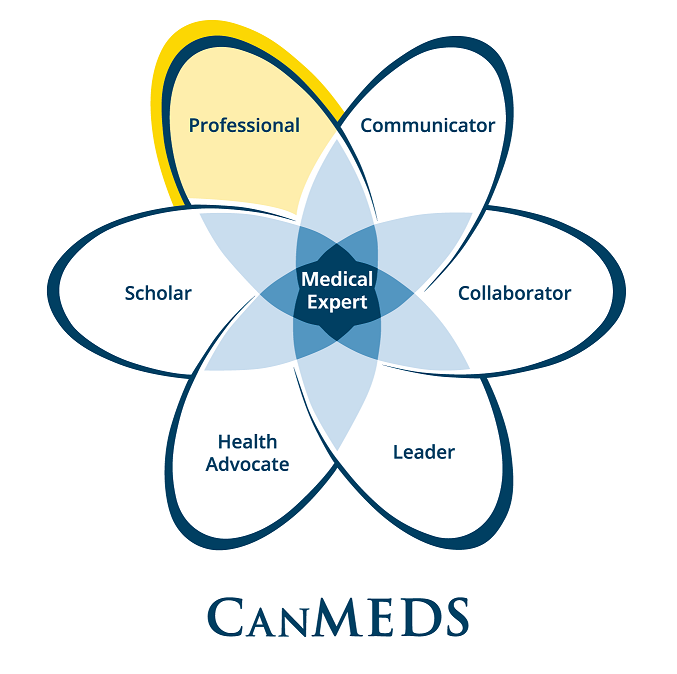
An environmental scan of existing physician health programming across Canada reveals that significant energy, commitment and activity is being directed toward physician health and wellness, but in many cases, efforts are siloed, under-resourced and piecemeal. The Physician Wellness Task Force has developed and a series of aligned with the existing CanMEDS Physician Competency Framework, that form a comprehensive guide for future work in the themed areas of Awareness and development, Sustainability, and Support.
What can I do now?
Program directors, residency program committee members, medical educators, health care leaders, resident physicians, medical students, accreditors, hospital administrators, wellness committee members and anyone else interested in physician wellness, can use the 15 recommendations with associated examples to guide the development or enhancement of local, regional or national initiatives that address the specific needs of medical learners and practicing physicians in different contexts and at every career phase.
What is the long-term goal for these findings?
Making systems change requires commitment from leaders and champions across all levels. The purpose of this report is to provide recommendations that will assist leaders, program directors and educators in implementing the physician wellness key and enabling competencies of the Professional Role, in practical and actionable ways, in their clinical and learning environments. Focusing on practical and actionable strategies for programming will enable the development of measurable outcomes. This in turn could inform the creation of future accreditation standards. The potential to influence accreditation standards holds promise for a more radical paradigm shift in the way that the health care system approaches physician wellness.
The Royal College would like to thank the following individuals for their assistance in developing this resource:
Dr. Leslie Flynn, Dr. Erica Dance, Dr. Caroline Gérin-Lajoie, Dr. Amber Hastings-Truelove, Dr. Mithu Sen, Dr. Christopher Simon, and Dr. Sarah Smith
Executive summary
Physicians are at high risk of experiencing adverse effects on their health and well-being, including burnout, depression and suicide. Such outcomes have implications for physicians, patients and health systems, with links to compromised patient satisfaction, medical errors and increased resource use. In 2005, Royal College Fellows made a lasting commitment to physician health and wellness when they added it to the CanMEDS Physician Competency Framework. The strategic addition of physician wellness competencies means that all residents of Canadian programs must develop important skills that can help to see them through their practice careers. Since the 2005 addition and the subsequent revision of the enabling competencies within the Professional Role in 2015, the Royal College, along with its many partners in medical education, has continued to support the development of a culture of wellness in medicine. The work of the Physician Wellness Task Force is a recent example of an ongoing and strong commitment to the wellness of physicians in Canada. This report on the Task Force’s work is in alignment with the 2015 enhancements of these enabling competencies within the Professional Role.
An environmental scan of existing physician health programming across Canada reveals that significant energy, commitment and activity is being directed toward physician health and wellness, but in many cases, efforts are siloed, under-resourced and piecemeal. By looking at the bigger picture, in Canada and internationally, the Task Force has developed a series of 15 recommendations that form a comprehensive guide for future work.
These 15 recommendations will enable the implementation of the physician wellness key and enabling competencies of the Professional Role in practical and actionable ways. This focus on practical and actionable strategies provides an opportunity to influence the creation of future accreditation standards and, in turn, shift the way that the health care system approaches physician wellness.
The hope is that the Task Force’s five guiding principles and 15 evidence-informed recommendations with associated examples will be used by program directors, residency program committee members, medical educators, health care leaders, resident physicians, medical students, accreditors, hospital administrators, wellness committee members and anyone else interested in physician wellness. They are meant to guide the development or enhancement of local, regional or national initiatives that address the specific needs of medical learners and practising physicians in different contexts and at every career phase.
Introduction
Physicians are at high risk of experiencing adverse effects on their health and well-being, including burnout, depression and suicide. Such outcomes have implications for physicians, patients and health systems, with links to compromised patient satisfaction, medical errors and increased resource use. Medical school and residency training are particularly challenging times; however, it is crucial to recognize that issues can emerge at any stage of training and practice. Factors that influence wellness occur at the level of the individual, the professional culture, the workplace, the organization and the system. Many of these factors are compounded by rising work demands and increasingly complex training and practice environments. Physician health and wellness is an emerging quality indicator, and it is critical that leaders, educators and other stakeholders address it across the career life cycle.
Many stakeholders have recognized these critical issues and have been attempting to find approaches and solutions to address them. All too often they have been working in silos, with limited resources, and without an evidence-based road map that is aligned with existing frameworks (e.g., the CanMEDS Physician Competency Framework). For meaningful improvements to be achieved in Canada’s physician health and wellness landscape there must be practical and actionable recommendations. These recommendations must emphasize the shared responsibility of the profession, the learning and clinical environments, the health system, as well as individuals to commit to promoting behaviours and training and practice conditions that optimize health and wellness.
Given the complexity of physician health and wellness and the range of contexts in which physicians learn and work, it is not surprising that there is no agreed-upon, overarching definition of physician wellness. This lack of definition has been one of the many challenges that have made it difficult to coordinate efforts at the local, provincial and national levels to improve key outcomes. To provide a reference point within which to ground the Task Force’s recommendations, and to promote consistency, we have broadly conceptualized health and wellness according to the CMA Policy on Physician Health (2017),1 as :
… [encompassing] the prevention and treatment of acute or chronic issues of individual physicians, as well as the optimization of interconnected physical, mental and social factors to support health and wellness. Attributable to a range of personal, occupational and system-level factors … [addressing] physician ill-health is being increasingly understood as a set of risk-management practices, including the use of strategies rooted in organizational psychology and occupational medicine, as well as intensified oversight by professional bodies, and the integration of maintaining personal health as a core medical competency.
As identified in one of the earliest contemporary definitions of physician wellness published in The Lancet (2009), it is also important to view physician wellness not only as the absence of illness but also as the capacity for physicians to thrive in their personal and professional lives.2 For a more comprehensive view of the physician health and wellness landscape in Canada, refer to the background document to the CMA Policy on Physician Health.3
The context
Despite the increased focus on physician wellness as a priority in Canada, there is a lack of standardized guidelines on this important component of competent professional practice. This has implications for medical educators and learners, medical practitioners, medical leaders, health care administrators, regulatory authorities and provincial and national governing bodies. To address this gap, the Royal College of Physicians and Surgeons of Canada formed a Physician Wellness Task Force to develop expert-informed, evidence-based guidelines and recommendations on standards for physician health and wellness for medical education and practice throughout the physician career cycle. This work aligns with the CanMEDS 2015 Physician Competency Framework,4 which identifies and describes seven Roles that are integral to optimal physician performance, care delivery and health care outcomes. In this framework, a key competency of the Professional Role is that “ Physicians are able to demonstrate a commitment to physician health and well-being to foster optimal patient care. ” The enabling competencies for this key competency establish the expectation that physicians are able to:
- exhibit self-awareness and manage influences on personal well-being and professional performance,
- manage personal and professional demands for a sustainable practice throughout the physician life cycle and
- promote a culture that recognizes, supports, and responds effectively to colleagues in need.
The purpose of this report is to provide recommendations that will assist leaders, program directors and educators to implement the physician wellness key and enabling competencies of the Professional Role, in practical and actionable ways, in their clinical and learning environments. Focusing on practical and actionable strategies for programming will enable the development of measurable outcomes. This in turn could inform the creation of future accreditation standards. The potential to influence accreditation standards holds promise for a more radical paradigm shift in the way that the health care system approaches physician wellness.
Making systems change requires commitment from leaders and champions across all levels of the organization. This goal and these competencies intersect with multiple aspects of the Leader Role. These include the key concepts of contributing to the development and delivery of continually improving health care, demonstrating leadership in professional practice, and managing one’s practice to maintain a sustainable practice and one’s personal health.
Guiding principles
A set of five guiding principles informed the recommendations and best practice guidelines presented in this report. These define the shared values of health care providers and can be used to inform decision-making and shape the culture of physician wellness. We have used these principles to write our recommendations and encourage others to adopt them within their own organizations and practices.
- Physician wellness is an essential and evidence-based aspect of medical education, practice and quality patient care.
- Physician wellness is important in all phases of the physician career life cycle, from medical school through to retirement.
- The responsibility for physician wellness is shared by the medical profession, individual physicians and medical learning and practice environments.
- Physician wellness requires commitment and engagement from stakeholders across the entire health care system to optimize physician health and well-being.
- Physicians have a collective responsibility to communicate when experiencing difficulties and to listen with support and without judgment when colleagues reveal that they are struggling.
Methodology
The Task Force undertook multiple steps to build and refine its recommendations. These included:
- Regular meetings of the Task Force in person and virtually
- An environmental scan of wellness programming at Canadian medical schools for learners and faculty as well as existing wellness resources available through provincial and national physician organizations
- The development of a template to categorize information about existing and aspirational physician health practices in Canada
- A scoping literature review of evidence-based practices in physician health published between 2010 and 2018
- Repeated surveys with stakeholders including meetings with the Advisory Committee and the presentation and workshopping of draft recommendations at two international medical conferences in the fall of 2018
- A 2021 review of recommendations to include examples relevant to the COVID-19 pandemic and its challenges
For a more fulsome look at this methodology and how it was guided theoretically by Brynjolfsson and colleagues’ matrix of change,5 please refer to Appendix A.
Getting most out of these recommendations
Intended users
The recommendations in this report are likely to be used by a range of people including program directors, residency program committee members, medical educators, health care leaders, resident physicians, medical students, accreditors, hospital administrators, wellness committee members and anyone else interested in physician wellness. Some people will work alone to improve physician health and wellness, and some will work together; either way, all should find something tangible within these recommendations to help them to make progress in reaching their goals.
For a more fulsome look at how to use this report, please refer to Appendix B.
Implementing change in complex environments
Health care systems are extremely complex, which means that changes to improve physician health and wellness require leadership and commitment on both a personal and organizational level if they are to be truly effective. The best outcomes are achieved when there is a balance of programming focused on affecting the profession and culture of medicine, the environments where physicians learn and work, and the individual practitioner.
Anyone looking to implement these recommendations should consider the dynamic interrelations among the personal and environmental factors that influence the culture of medicine and more specifically the culture of wellness. Similarly, when implementing these recommendations, one needs to consider creating and/or updating appropriate policies, protocols, programming and resources to ensure that the recommendations will lead to lasting improvements.
Recommendation structure — Building in the CanMEDS Professional Role
The physician wellness competencies were critical to the development of recommendations. Any recommendations that were not in alignment with these competencies would be irrelevant to postgraduate medical education and practitioners in Canada. The physician health key competency serves as the overarching goal for the recommendations: Physicians are able to demonstrate a commitment to physician health and well-being to foster optimal patient care. There are three sections of recommendations, which correspond to the three enabling competencies in the 2015 CanMEDS Framework. These enabling competencies were analyzed to elicit the essential themes.
The first enabling competency, Physicians are able to exhibit self-awareness and manage influences on personal well-being and performance, evoked two themes: the need for building awareness and the need for skill development.
The second enabling competency speaks to sustainability and the maintenance of wellness. Physicians are able to manage personal and professional demands for a sustainable practice through the physician life cycle. This competency requires physicians to be able to recognize factors that influence wellness and to utilize the awareness, knowledge and skills they have acquired.
The third enabling competency identifies that support will be required for individuals who are in distress, unwell or in crisis. Physicians are able to promote a culture that recognizes, supports and responds effectively to colleagues in need. Moreover, this competency specifically addresses the need for this to occur not only at an individual level of peer-to-peer support but also at the level of the profession.
For each recommendation there is a list of specific ideas or examples on how a program or institution could implement the recommendation. These examples are not meant to be prescriptive or exhaustive. Think of each list as starting with the statement “programming to fill this recommendation may include but is not limited to the following examples.” Programs may choose to use some or all of these examples or find others that are more appropriate for their program. The goal is to meet the recommendation; the route that individual programs take to get there is up to them.
For example, consider a program director who is seeking information on how to help residents who are thriving in the program to maintain their current level of wellness. Specifically, this program director would like to help their residents "Manage personal and professional demands for a sustainable practice throughout the physician life cycle." The program director looks in the Sustainability section and notes that one of the recommendations is "Promote sustainable practice by creating policies, processes and strategies to facilitate flexibility in training and work." The examples listed for this recommendation are flexible scheduling, leave policies, working from home and time to go to health care appointments. The program director knows that their university already endeavours to make schedules well balanced and fair and has robust processes around leaves of absence. But they realize that few residents request time off for medical appointments, which makes them wonder whether there is a strategy in place for how a resident may do this and whether this kind of request is supported by the culture in which the resident works. To address this, the program director schedules a meeting with residents to get feedback on this question and then works with the residency program committee to create a plan to ensure that residents have the support they need to attend medical appointments periodically throughout the year.
Local implementation
The recommendations and ideas or examples are not a checklist or a recipe. Instead, they are meant to support the creation and maintenance of locally relevant educational and practice environments. There are variations in programming and policies for physician wellness among schools, programs within those schools, and other organizations, and as a result different sites may have different needs for change. Many of these recommendations and examples are already well engrained in some clinical and learning environments, whereas other recommendations and suggestions will be new and/or challenging for some institutions to adopt. Users should celebrate their accomplishments in cases where recommendations have already been met and then focus their attention on the unmet recommendations that are most relevant to their population(s). These recommendations should be useful for both training and practice environments as they address wellness issues throughout the physician life cycle.
Programming as an ongoing commitment
Of note, the word “programming” is repeatedly used in these recommendations. This word was deliberately chosen to ensure that the implementation of a recommendation involves providing not simply a didactic session, but rather a toolkit of activities and learning experiences in a variety of settings, for a variety of participants. Meaningful change rarely comes from a “one and done” approach. For this reason, these recommendations are written to encourage ongoing efforts.
Recommendations at a glance
The 15 recommendations of the Task Force are presented in an at-a-glance format in the following table.
In this table there are examples of how the recommendations could be achieved by individual programs, departments and organizations. The Task Force chose examples grounded in the literature and in expert endorsement, but the list is not exhaustive. The Task Force recognizes that every institution and educational program is unique and that implementation will need to be tailored to the institution or program’s individual context.
| Key dimension 1 | Recommendation |
|---|---|
| Awareness |
|
| Development |
|
| Sustainability |
|
| Support |
|
- These key dimensions are rooted in the physician wellness competencies of the Professional Role.
- Note: the term "programming" is used to describe a toolkit of activities and learning experiences in a variety of settings, for a variety of participants.
Recommendations 1 to 6: Awareness and development
The following six recommendations relate directly to Professional Role enabling competency 4.1: Exhibit self-awareness and manage influences on personal well-being and professional performance.
The themes acknowledge the separate, but complementary, importance of education to build awareness and the need for skill development.
Recommendations for awareness
Develop and implement educational programming to build awareness around physician wellness at every stage of the physician life cycle
Programming may include the following topics:
- Decreasing stigma
- Acknowledging and addressing power dynamics
- Appreciative inquiry
- Motivational techniques
- Principles for wellness (i.e., autonomy, control, learning, connectedness, aspiration, meaning, thriving, practice efficiency, civility, isolation, experience of care)
- Risks of the profession as whole and of specific specialties
- Health-related policies (e.g., accommodations)
- Existing resources available to support wellness
- Identifying drivers of influence
- Identifying existing resources
- Identifying individual needs
- Needs assessments
- Positive psychology
- Emphasizing lifelong learning
- Core values of compassion
- Recognizing implicit biases
Develop programming to raise awareness about systemic issues influencing physician wellness
Programming may include the following topics:
- The Quadruple Aim
- Cultural safety
- Equity, diversity and inclusivity
- Professional behaviours in the workplace (e.g., boundaries, delivering and receiving care, delivering and receiving feedback)
- Physical and psychological safety
- Results of a workforce survey
- Challenging the status quo — adverse events
- Workforce (Areas of Worklife Scale)
- Quality and practice improvement initiatives
Implement processes that measure and evaluate the state of wellness of medical learners and faculty
Programming may include the following examples:
- Measuring wellness (e.g., survey tools)
- Identifying drivers of influence
- Consistency in use of evaluation tools
- Consistency in use of definitions
- Consistency in wellness initiatives
- Practice improvement models
- Encouraging self-assessment (decreasing stigma)
Recommendations for development
Implement educational programming to teach skills to promote a culture of wellness in the clinical and learning environments
Programming may include the following topics:
- Team roles and dynamics
- Responding to adverse events
- Peer support training
- Creating a wellness committee
- Creating opportunities for community building and social support
- Managing difficult patient encounters
- The impact of poor physician health on patient care
- The impact of poor physician health on professional performance
- How to be a patient
Develop programming to teach advanced leadership skills in physician wellness
Programming may include the following topics:
- Critical communication
- Providing psychologically safe feedback
- Establishing boundaries
- Recognizing distress
- Training physicians on caring for physicians
- The impact of poor physician health on patient care
- Costs of poor physician health
- Compassionate leadership concepts
Develop programming to teach skills to enhance wellness for the individual
Programming may include the following topics:
- Nutrition
- Coping with moral distress
- Fatigue risk management
- Physical wellness
- Mental health
- Time management
- Self-reflection
- Mindfulness
- Resilience
- Managing technology
- Meditation
Recommendations 7 to 11: Sustainability
The following five recommendations relate directly to Professional Role enabling competency 4.2: Manage personal and professional demands for a sustainable practice throughout the physician life cycle.
Programming related to this competency addresses the sustainability and maintenance of wellness. Interestingly, this competency requires physicians to be able to recognize factors that influence wellness and to use the awareness, knowledge and skills they have acquired (recommendations 1–6).
Recommendations for sustainability
Promote sustainable practice by creating policies, processes and strategies to facilitate flexibility in training and work
Programming may include the following examples:
- Flexible scheduling
- Leave policies
- Working from home
- Time to go to health care appointments
Make tools and educational programming available to enable physicians to manage personal and professional demands
Programming may include the following examples:
- Managing self-care
- Available peer support
- Employee assistance programs
- Human resources entitlements
- Electronic medical record (EMR) training
- Managing transitions
- Financial planning
- Managing work–life balance
- Recognizing personal distress
- Consulting with others regarding personal wellness resources
- Maintaining healthy interpersonal relationships
- Self-audits for wellness
- Creating and practising professional boundaries
- Managing social media appropriately
Acknowledge and support wellness initiatives and programs
Programming may include the following initiatives:
- Creation of wellness champion positions
- Wellness leader awards
- Continuing professional development (CPD) or continuing medical education (CME) credits for participation in CPD offerings
Make resources that support wellness of all physicians available and easily accessible
Programming may include the following initiatives:
- Healthy nutritious food available 24 hours per day
- Access to childcare
- Access to a quiet room for prayer, sleep, fatigue management, breast-feeding
- Access to a family physician
- Access to confidential counselling services
- Access to a physician lounge
- Access to an onsite gym or opportunities for physical activity
- Access to parking
Encourage leaders to promote and create a culture of wellness
Programming may include the following initiatives:
- Recognizing wellness champions
- Awards for implementing wellness initiatives
- Requiring a commitment to wellness as a component of leadership roles
- Positive affirmations
- Including wellness in the strategic plan
- Including wellness as an agenda item for meetings
- Setting controlled hours
- Creating wellness retreats
- Creating a nonjudgmental atmosphere
- Creating space for social activities (e.g., birthdays)
- Creating a social committee
- Implementing a “kudos” box
- Building social community
- Coaching
Recommendations 12 to 15: Support
The remaining four recommendations relate directly to Professional Role enabling competency 4.3: Promote a culture that recognizes, supports, and responds effectively to colleagues in need.
This indicates that support is required for individuals who are in distress, unwell or in crisis. It specifically addresses the need for this support to be offered not only at the individual level of peer-to-peer support but also at the level of the profession.
Recommendations for Support
Make resources available to support and promote health and wellness
Programming may include the following examples:
- Financial advisors
- Career development and redirection counselling
- Physician wellness leads
- Mentoring and coaching
- Access to peer support persons and/or groups
- Access to family physicians
- Access to occupational health
- Road to Mental Readiness program
Make resources available to support and respond to individuals in need
Programming may include the following examples:
- Availability of substance use counselling
- Linkages to provincial physician health programs
- Availability of mental health resources
- Access to confidential counselling
- Employee assistance programs
- Availability of family support
- Availability of early identification and intervention
Institute policies to support individuals in acute distress
Programming may include the following examples:
- Leave policies (e.g., leaves of absence)
- Established protocols to respond to adverse events
- Established practices to recognize and respond to colleagues in distress
- Established protocols to respond to physician suicide
Ensure policies and practices support flexibility in training and practice to meet varied needs and circumstances
Programming may include the following examples:
- Accommodations
- Flexible work and training schedules
- Modified training, work and call schedules
- Availability of job sharing
- Part-time training
Committee membership
This report is the culmination of work that would not have been possible without the participation of Canadian experts in physician wellness who were part of the Physician Wellness Task Force and the Physician Wellness Advisory Committee.
Both the Task Force and Advisory Committee were chaired by Dr. Leslie Flynn, vice-dean education of the Faculty of Health Sciences at Queen’s University and a clinician educator with the Royal College.
This project has been supported throughout by Megan McComb, a designated project coordinator at the Royal College, within the CanMEDS and Faculty Development team.
TASK FORCE
The Task Force was struck in 2017 to develop a Physician Wellness Strategy for the Royal College of Physicians and Surgeons of Canada to influence physician education in the competency-based medical education era and to advise the Royal College on the future configuration of residency education to promote wellness, including implications and standards for accreditation.
Task Force members were recruited specifically for their expertise and experience with physician wellness.
Task Force members:
Erica Dance, assistant dean, resident & fellow affairs, Office of Advocacy & Wellbeing, Faculty of Medicine & Dentistry, University of Alberta
Caroline Gérin-Lajoie, executive vice-president, Physician Wellness and Medical Culture, Canadian Medical Association
Amber Hastings-Truelove, health education researcher and consultant, Office of Professional Development and Education Scholarship, Faculty of Health Sciences, Queen’s University
Mithu Sen, acting vice dean, faculty affairs, Schulich School of Medicine & Dentistry, Western University
Christopher Simon, director, Physician Wellness and Medical Culture, Canadian Medical Association
Sarah Smith, resident physician, University of Toronto, and Resident Doctors of Canada
ADVISORY COMMITTEE
Members of the Advisory Committee were recruited for their expertise in physician health and/or their expertise and experience in education. They were consulted to provide their input and feedback on draft documents prepared by the Task Force. They also contributed to the final recommendations and report.
Advisory Committee members:
- Joy Albuquerque
- Shabbir Amanullah
- Meri Bukowskyj
- Craig Campbell
- Andrew Clarke
- Mamta Gautam
- Mackenzie Grisdale
- Joan Horton
- Michael Kaufmann
- Jane Lemaire
- Hamza Mahmood
- Christina Nowik
- Sandra Roman
- Nureen Sumar
- Miranda Wan
Conclusion
It is increasingly apparent that attending to the health and wellness of physicians is a shared responsibility of the profession itself, the organizations in which physicians are educated and practise, and individual physicians. Physician wellness issues affect every aspect of our health care systems: they have an impact on not only individual physicians but also physicians’ families, colleagues, work and learning environments, and patients. Awareness of the importance of physician wellness has been increasing. Joy Albuquerque and Dorian Deshauer argue that changes in the medical landscape are shifting the way that the profession looks at wellness. It is moving it from a private matter to “something closer to a shared resource.” 6 They suggest that in Canada, “three main mechanisms are driving this change: the use of risk-management strategies adapted from organizational psychology and occupational medicine to change physician behaviour, intensified oversight of physician health by professional bodies and the adoption of health itself as a core value in the medical profession.” They indicate that the CanMEDS Framework has played a role in this transformation. The Task Force members completely endorse this view and have employed a similar lens in their approach to this work. The Task Force explicitly identifies the need for policies, strategies, resources and programming that can create cultural change and that can promote wellness in work and learning environments as well as for individual physicians.
The intent is for this report to be used not only by those involved in residency education but also by wellness committees, hospital administrators and policy-makers to implement changes to measure, monitor and, if necessary, improve physician wellness in their environments. Recognizing that there are different accreditation standards for clinical and learning environments, this document may inspire those who can enact change to use these recommendations to inform future accreditation standards. Following Shanafelt and colleagues,7 organizational leaders are encouraged to find ways to engage and empower physicians to identify challenges to wellness in their organizations and work units and to support initiatives that foster wellness in their unique environments.
References
- Canadian Medical Association. CMA Policy on Physician Health. Ottawa: Canadian Medical Association; 2017.
- Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet2009;374:1714-21. Available: https://doi.org/10.1016/S0140-6736(09)61424-0.
- Canadian Medical Association. Background to CMA Policy on Physician Health. Ottawa: Canadian Medical Association; 2017.
- Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
- Brynjolfsson E, Renshaw AA, Van Alstyne M. The matrix of change.MIT Sloan Management Review1997;38(2).
- Albuquerque J, Deshauer D. Physician health: beyond work–life balance.CMAJ2014;186(13):E502.
- Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine program. Ann Intern Med2002;136(5):358-67.
APPENDIX A - METHODOLOGY
The Task Force adapted Brynjolfsson and colleagues’ matrix of change to guide the approach to this project. The four steps in their process were used to identify critical interactions between the various aspects of physician wellness and the multiple processes involved in supporting it:
Identify existing goals and processes: The initial step has two parts. First, existing goals and processes must be identified. The Task Force began by conducting an environmental scan of wellness programming at Canadian medical schools for medical students, residents and faculty, also looking at resources that were offered provincially and nationally.
Second, specific processes and goals need to be targeted for change. At this point, a wish list was compiled of what evidence-informed physician wellness programming could look like.
Look at system interactions: The second step in the matrix of change is to understand how existing practices fit together within larger systems. Three different levels of the medical system were considered: culture/profession, organization/environment and individuals. The Task Force thought about the elements within each level that influence physician wellness positively or negatively and also considered how these elements interact between levels. To organize the data that were collected, as well as the Task Force’s thinking, a template was crafted to capture the information the Task Force gathered for all three levels.
Identify transition interactions: In the matrix of change, transition interactions are the interactions involved in moving from existing to ideal practices. Recognizing that many medical schools and organizations are already working to implement physician wellness programming, the question was posed of what an ideal physician wellness curriculum could look like. A scoping review was conducted of the literature published between 2010 and 2018 to identify evidence-based best practices in physician wellness. The initial search yield 2178 results. After duplication was eliminated, 1907 articles were left. Next, papers that focused on patient wellness rather than physician wellness were eliminated, as well as papers from countries other than Canada, the United States, the United Kingdom and Australia), leaving 951 articles. Lastly, the Task Force excluded papers that did not have an abstract. The remaining articles were then divided thematically on the basis of their abstracts, further excluding editorials, articles that reported pilot data and papers focused on only one specialty or subspecialty. This left 156 articles.
By adding these articles to the template, as the recommendations developed the Task Force could visually identify which ones were substantiated by empirical data and therefore which ones were supported by the strongest evidence. For example, a number of articles have shown that wellness programs that include breathing techniques, meditation and relaxation exercises can improve the stress levels of medical students.
The goal in compiling this information was to create a single resource that bridges the existing work occurring across Canada with the wealth of evidence suggesting best practice possibilities for future physician wellness curricula and programming.
Survey the stakeholders: Hearing from experts in the field is the final step. The Advisory Committee provided important feedback to the Task Force at each stage of the work.
Further, at the International Conference on Physician Health and the International Conference on Residency Education, both in October 2018, the Task Force conducted workshops to crowdsource additional thoughts and suggestions. The attendees included many of the Task Force’s stakeholder groups, such as program directors, medical educators and learners, as well as international experts in physician health. From this considerable feedback, new suggested recommendations were added to the template to enhance it.